Что такое вирус вирджиния

Last updated on April 18 at 1:00 p.m.. E.D.T.
Virginia is reporting 8,053 confirmed cases of COVID-19, along with 1,296 people who have been hospitalized and 258 deaths, according to the Virginia Department of Health. That puts Virginia in the top half of states with U.S. coronavirus cases; it is the 12th most populous state. About 51,931 people have been tested.
Virginia also began listing the total number of outbreaks in the state; that currently stands at 129. Most, or about 74, of those outbreaks occurred in long-term-care facilities, 22 occurred in "congregate" settings, 16 in healthcare settings, 11 in correctional facilities, five in educational settings and one in another, unspecified setting.
People of every age are testing positive for the disease, but most deaths and hospitalizations are occurring in those over age 40. About 71% of cases are occurring in those over age 40, while 89% of hospitalizations have occurred in those over age 40 and 99% of deaths have occurred in those over age 40. One person in their 20s, and two in their 30s have died of the virus.
Latest updates
—On Friday (April 17) Gov. Ralph Northam said the state's rising case count suggested it was not yet ready to reopen. "Just like everybody, I want to get back to being as near normal as we can as soon as possible, but we have to be patient," Northam said during a coronavirus news briefing. Among the criteria required before reopening is feasible: a consistent decrease in case counts for 14 days, and enough testing supplies and contact tracing infrastructure to quickly identify and isolate new cases once they occur, Northam said.
—On Wednesday (April 15) Gov. Ralph Northam announced an extension of executive order 53, which closed nonessential businesses and mandated social-distancing guidelines for those that remain open. The updated order is in effect until May 8.
—About 65% of all known COVID-19 cases in the state are tied to distinct clusters of local transmission, according to WTVR.
—Virginia received a new shipment of personal protective equipment, Northam announced on Wednesday (April 8). The state will receive 1.5 million pairs of gloves and 430,000 N95 masks, NBC12 reported.
—Virginia's total COVID-19 count likely represents a significant undercount, due to limited testing, the Richmond Times-Dispatch reported. For instance, a dashboard that tracks local hospitalization, run by the Virginia Hospital and Healthcare Association (VHHA), notes at least 1,287 people being treated for COVID-19 in the state's hospitals, with another 721 who have been discharged already. The total number of reported cases, at 3,333, is roughly three times the total number of people known to be hospitalized in the state. Because around 80% of COVID-19 cases are thought to be mild and not require hospitalization, there are likely many more undetected cases in the community. Currently, 4228 people are in intensive care units and 276 are on a ventilator, according to the VHHA dashboard.
—Virginia will begin using genetic testing to analyze samples of SARS-CoV-2 taken from patients in the state. This genetic sequencing will allow researchers to trace the origin and spread of the disease. Genetic analysis will also allow researcher to track whether the virus is mutating, or changing, in significant ways. So far, studies suggest the SARS-CoV-2 virus mutates much more slowly than the influenza virus.
—The University of Virginia is enrolling patients in a clinical trial of an experimental antiviral treatment, remdesevir, made by Gilead Sciences. The trial will enroll 440 people worldwide who are hospitalized with severe COVID-19, to see if the antiviral drug improves their outcomes.
—The Army Corps of Engineers is surveying the state for 41 potential sites of makeshift hospitals. Some candidates include the Exxon Mobil facility in Fairfax, the Hampton Convention Center and a yet-to-be-announced site in Richmond, NBC12 reported.
RICHMOND, Va. (AP) — Ronald Mitchell worried about his mother’s care at a suburban Richmond nursing home long before she was swept up in one of the nation’s deadliest coronavirus outbreaks.
She’s bedbound and susceptible to seizures. A sore on her foot went unnoticed for so long, he said, that it led to the amputation of her leg. When he called her last month after she tested positive for COVID-19, she sounded disoriented, and he stayed on the line as she pressed a call button and waited an hour and a half for a nurse who never came.
Mitchell then called Canterbury Rehabilitation & Healthcare Center directly and was told that they were doing the best they could with just two nurses looking after 40 patients at a time in the coronavirus quarantine wing.
With the death toll from the Canterbury outbreak rising to 45, Mitchell can only hope that his 62-year-old mother now on a ventilator in a hospital won’t be next.
“It’s the worst feeling in the world,” he said.
Canterbury, which has surpassed the death toll of 43 in the outbreak at the Life Care Center in suburban Seattle, is the kind of facility that’s particularly vulnerable to a coronavirus wildfire that has raged through the nation’s frail, elderly long-term care populations, claiming more than 4,300 lives.
Nearly all of Canterbury’s residents rely on Medicaid funding for care of health problems that in many cases were the product of a lifetime of poverty. It lacks the amenities and space to keep people apart. And it lacks the pay to hire and keep enough staff.
“A publicly funded nursing home is a virus’s dream,” said Dr. Jim Wright, Canterbury’s medical director. “It is the best place for a virus to be. People are close together. Their immune systems are compromised. It is just a tinderbox for that match.”
Studies have shown nursing homes heavily dependent on Medicaid for revenue have fewer nurses and other staff per patient than average and lower quality of care overall. And some of the biggest outbreaks so far have been at homes tied closely to the government payment program, including ones in Wayne, West Virginia, and the Crown Heights section of New York City’s Brooklyn borough.
Canterbury, which had about 160 residents before its outbreak, was thrown into turmoil from the first COVID-19 diagnosis on March 18. Many of the staff who work at multiple facilities — Wright couldn’t say exactly how many — quit because they otherwise wouldn’t have been able to continue at their other jobs. Other workers began to get sick themselves.
Around the same time, the second doctor who typically saw patients just stopped showing up, which Wright said had a severe impact on the ability to monitor patients. His wife, a palliative care physician, started volunteering. Everyone at Canterbury had no choice but to take on unfamiliar tasks.
“I was changing patients, cleaning beds. My administrator was delivering meal trays,” Wright said.
“You pick any element, or any arena in our facility that needed to be up and running at its best and nothing was,” he said.
Exactly how the coronavirus got into Canterbury was not clear, though health officials suspect either an infected worker or someone else who came in before visitations and get-togethers were halted in mid-March.
COVID-19 tests were available but scarce at the beginning of the outbreak, but Canterbury was not initially able to test all of its residents and staff because of guidance from state and national officials at the time. Virginia’s rules said even long-term care residents had to first be tested to rule out the flu and other respiratory pathogens, something Wright and other medical directors asked the health department to change because of the delay it created.
By the time tests were finally conducted on everyone at Canterbury about two weeks after the first confirmed case, more than half the residents infected with coronavirus — 53 out of 92 — showed no symptoms of the disease.
“It’s impossible to build walls around something that spreads so insidiously,” said Dr. Danny Avula, the state health department’s area director who has noted that Canterbury has been doing its best.
Even in normal times, Canterbury merited just one out of five stars in Medicare’s rating system, with inspection records showing the facility had such poor staffing levels that it impacted patient care.
One nurse told an inspector last year “residents would stay in bed because it is almost impossible for two people to assist 62 or 63 residents.” Previous inspections also found infection-control problems and failure to report an attempted rape of a patient.
Relatives of Canterbury residents described a facility with long-running quality-of-care problems and said they thought more could have been done to prevent the spread. They also said they had not received adequate communication during the crisis.
Kim Thompson’s phone rang before 6 a.m. Thursday, and when Wright told her that her 72-year-old mother, Minnie Brown, had died, she thought it had to be a mistake.
Thompson had spoken with her mother over FaceTime two days earlier and she seemed in good health and spirits. Since that phone call, the family had received no updates from Canterbury letting them know her condition had deteriorated.
“It’s neglect. It’s negligence,” Thompson said in an interview.
Thompson said as Canterbury’s death toll began to climb, she started researching the response at the Life Care Center outbreak near Seattle, where a special federal group of doctors and nurses was sent to help.
Since then, several governors have used their emergency power to do the same for their homes. The National Guard was called in to evacuate a home in Tennessee, take over another one in Massachusetts and run tests at a third in Wisconsin. And special “strike teams” have been tapped to run tests and ferry supplies to homes in Ohio, Indiana and Maryland.
“Where is the state in some of this? Why wasn’t more done on a state level as well to come in and take over the situation?” Thompson asked, noting that at one point the victims from Canterbury accounted for about a third of the state’s dead. “There’s lots of blame to go around.”
Virginia Gov. Ralph Northam recently proposed a budget amendment that increases the rates paid to nursing homes and long-term care facilities by an additional $20 for Medicaid recipients per day. He’s also announced the creation of a task force that is working with such facilities to try and cut the infection rates and deaths.
“This boost in funding will help these facilities address staffing issues during this epidemic,” Northam said.
Wright, who continues to care for the Canterbury patients who remain, was asked in a news conference last week if he would have done anything differently.
“I would have a nursing home that had enough staff around-the-clock, around all the time. I would have a nursing home where everyone had private rooms. I would have a nursing home where there was greater access to the outdoors,” he said.
“In other words, I would have a nursing home funded by a society that puts more emphasis on treating our elders the way they should be treated.”
Condon reported from New York. News researchers Randy Herschaft and Rhonda Shafner in New York contributed to this report.
When inside-the-box thinking doesn’t cut it, you need to get out of it.
Staff at the University of Virginia Medical Center threw away convention to find a way to extend the life of personal protective equipment in the face of the highly communicable and deadly virus, SARS-CoV-2.
With a pandemic raging, staff across the center’s departments worked to find ways of extending the life of protective gear as shortages of N-95 masks and other equipment used when treating patients grew critical in other parts of the country struck by COVID-19, the disease caused by the virus.


Staff wound up playing McGyver with a robot designed to clean hospital rooms of virulent organisms, turning it into a virus-killing, gear-cleaning, ultraviolet ray gun called Tru-D.
There was a need for speed. Dr. Carlene Muto, assistant professor of infectious diseases and international health, had been on a trip to Italy with her daughter when the pandemic began to ravage that country.
“We got out in the nick of time and I started thinking, ‘What’s going to happen when it gets here?’” Muto recalled.
“For us, the problem was not the protective gloves or gowns but the masks. There are different types and people who fit in one type can’t necessarily fit into another,” she said. “Normally, we don’t reuse them but when there’s a shortage of them around the world and the (Centers for Disease Control and Prevention) is putting out advice on reusing them, we knew we had to address it.”
With advance warning, Muto said medical center management was willing to get behind anything that could make supplies last longer.
There were options. Some hospitals use a hydrogen peroxide electrostatic misting device to kill resistant bacteria and pathogens in patients’ rooms and have modified that to kill the new coronavirus.
But, according to industry research, proper use of the equipment takes time, training and calibration.
“Then there was ultraviolet light,” Muto said. “It’s been used in health care for decades. We were already using it to disinfect equipment.”
In her previous stint at the University of Pittsburgh Medical Center, Muto had seen equipment like the robot used to disinfect patient rooms. The robot’s name, Tru-D, is short for Total Room Ultraviolet Disinfection.
The robot is effective at killing various organisms including Clostridioides difficile, typically known as C. diff., an antibiotic-resistant bug that can cause severe illness and even death and often is caught while in a hospital.
Tru-D’s operation seems simple. It stands in the room’s center, using sensors to calibrate the exact dose of energy necessary to disinfect the entire room. It turns on its light. The light is reflected back so all surfaces receive the right amount of power.
You can’t see it happen, but the high-energy light is absorbed in the cellular RNA and DNA of microorganisms, damaging nucleic acids to prevent them from reproducing. Pretty much neutered, the organisms no longer can infect humans and die without replicating.
Muto met with others and discussed the options. If Tru-D could kill the coronavirus in a room, could it kill the virus on protective gear within a room?
“We were using it in Pittsburgh to disinfect patients’ rooms,” Muto said. “Some of those gizmos can be set to a high level of energy and kill C. diff spores, which are hard to do. We had some UV machines here, but they didn’t have the 360-degree sensors needed to clean a whole room. It seemed like it would be the easiest to just drop into place.”
What normally would have taken a while to propose, study, arrange, purchase, deliver and set up was accomplished in a very short time.
“Our leadership was on it and they understood the issue and how little time we had to act,” Muto said. “We have been pushed to a place where merely purchasing the best products is no longer an option because there are none to purchase. There is a worldwide shortage and hospitals and states and countries are trying to purchase gear. There has never been a more crucial time, or a need so great to become a thinker out of the box. We need to think, plan and do. “
And so they did.
Epidemiology, clinical engineering, procurement, clinical staff, environmental services, supply chain staff, central sterile processing teams and senior leadership teams went to work.
A classroom was repurposed for a sterilization chamber. Its surfaces were painted with reflective paint to increase Tru-D’s efficiency.
With a chamber in hand, engineers designed racks to go into the room that could hang gear at the right distance and angles to make sure no piece of virus would miss its dose of radiation. Special collection boxes were designed so that the masks could be brought to the sterilization chamber without shedding any virus along the way.
Management then approved purchase of the 5-foot, 6-inch tall device.
The problem was that it could take several weeks, like a dozen, to deliver. Channeling Radar O’Reilly from the television show MASH, Muto reached out to a friend that could make it happen much quicker.
“In Pittsburgh we had about 30 of those things in different hospitals and clinics so I knew someone at the company,” she admitted. “I talked to him and we were able to find one. Management quickly got us a purchase order and it was going to be shipped. Except that it would take three weeks.”
That, everyone agreed, was too long.
“They said ‘if you come and get it, you can have it now.’ So we did,” Muto mused.
Michael Friesen, director of clinical engineering, and Patrick Headley, manager of clinical engineering professional services, grabbed the keys to the company plane and traveled to Tennessee to get training, get the machine and get home.
“The robot is large, fragile and incredibly valuable, yet we needed to get it operational as quickly as possible,” said Friesen.
“This is truly an all-hands-on-deck situation, and every hour and day is important,” Headley said. “We were on our way Monday morning, returned home that afternoon with Tru-D in hand and had the robot’s UV light up and running by Tuesday afternoon.”
Set at maximum power, Tru-D can disinfect hundreds of masks with each 20-minute cycle. Total cycle time from prepping the prep masks to disinfection, recovery and repackaging for the frontline healthcare providers is a little less than an hour for about 6,000 masks a day.
“By utilizing Tru-D, we can extend our current supply of personal protective equipment to meet the essential needs of our frontline faculty and staff,” said Dr. K. Craig Kent, executive vice president for health affairs. “UVa Health will continue to do all we can, from supply chain management to clinical innovations, to ensure every person in our facilities is safe and protected.”
Muto said she is proud to have played a role in the innovative, off-the-cuff and out-of-the-box thinking that put the medical center ahead of a potentially life-threatening problem.
“It’s the kind of thinking we need right now. We have never in our lives been faced with anything like this and drastic times require drastic measures,” she said. “It’s really forced people to be innovative thinkers. There has never been a time where the need was so great. I’m proud of the people here. We don’t wait. We get it done. I’m proud to be part of that.”

The Associated Press
April 17, 2020, 5:46 PM










ANNAPOLIS, Md. (AP) — Long linked by proximity and the hundreds of thousands of federal workers who live and work in their jurisdictions, Maryland, Virginia and the District of Columbia are now connected by the growing numbers of coronavirus cases they are battling.
Maryland Gov. Larry Hogan, Virginia Gov. Ralph Northam and District of Columbia Mayor Muriel Bowser spoke in a conference call Friday to discuss coordinating virus response efforts. Hogan said the three officials have frequently spoken over the past month. Hogan also noted that their staffs are in daily contact.
“While we may have individual differences about how we’re going after different things, the sharing of information, the willingness to try to cooperate on things that are of importance to the region has been terrific, and it has been throughout the crisis, and I think it’s going to continue,” Hogan said Friday after the call.
Hogan noted that this was the deadliest week yet in the region in and around the nation’s capital. He said the area has had more than 21,000 cases of coronavirus and 818 deaths.
As states review guidelines from the White House aimed at easing restrictions in areas with low transmission of the coronavirus, cases in areas near the capital are “going up rather than down,” said Hogan, who is the chairman of the National Governors Association.
“We’re all in some part of a phase of talking about the gradual reopening but not able to start that quite yet, and we all are in agreement that we want to do that in a way that’s cooperative,” said Hogan, a Republican. “We understand that while each area is unique that there are certainly things that we have to do together as a region.”
Northam, a Democrat, said at a news conference Friday that Maryland, Virginia, North Carolina and the District would “do everything that we can to be in coordination and be consistent” when it comes to reopening the economy.
“We share some of the same challenges, and we will do everything that we can to be in coordination and be consistent so we’ll be as straightforward as possible for everybody in this region,” Northam said.
Northam said he, Hogan and Bowser had discussed coordinating regionally on when to lift restrictions on elective surgeries.
“We want to be consistent because what we don’t want to happen is, if we do it sooner in one state than the other, then individuals will go to other states to have their surgery done,” Northam said.
Northam said Virginia does not meet the criteria to start even the first phase of the White House plan. To do so, the state would need its number of positive tests to be on a downward trend for 14 days.
“We have not met that criteria. We’re still seeing more cases each day, not fewer. So we are not there yet,” he said.
Governors in the Northeast and along the West Coast this week announced separate state compacts to coordinate how to begin reopening society amid the coronavirus pandemic. They did not announce specific plans on how to scale back stay-at-home orders or reopen businesses. Instead, both groups said they would coordinate those decisions while first considering the health of residents.
Although Hogan, Northam and Bowser have not been as formal in announcing a compact, they have been working together for weeks. For example, the three signed a letter to President Donald Trump dated March 15, requesting that the president add the region as a priority location for a federally supported testing site.
“The National Capital Region is home to over six million residents and the seat of the federal government, with hundreds of thousands of employees and contractors serving the Department of Defense and other mission essential agencies,” the three wrote. “The health of the National Capital Region is a top priority for the continuity of our democratic government and critical to continuing federal government functions.”
For most people, the coronavirus causes mild or moderate symptoms, such as fever and cough that clear up in two to three weeks. For some, especially older adults and people with existing health problems, it can cause more severe illness, including pneumonia and death.
Associated Press writer Sarah Rankin contributed to this report in Richmond, Virginia.

April 16, 2020, 9:30 AM
The novel coronavirus has swept through the D.C. area, spurring massive changes in the way we live our lives — from whether we go to work to how our children are educated.
Below is a timeline of some of the key developments over the past few months.
WTOP will continue to update this timeline as things change.

In this Jan. 30, 2020 file photo, a man wears a face mask as he stands along the waterfront in Wuhan in central China’s Hubei Province. (AP Photo/Arek Rataj, File)
Reports first emerge of a mysterious pneumonia-like illness linked to an outdoor food market in the Chinese city of Wuhan.
Doctors and scientists studying the illness determine the viral pneumonia is caused by a new type of coronavirus, according to reports in Chinese state media.
At that time, 59 people had contracted the illness, local authorities said. Later that month, the entire province is locked down. The lockdown would last 76 days.
The U.S. confirms the first known cases of the new coronavirus in the country: five cases in Washington state, all among people who traveled to the Chinese city at the center of the outbreak.

This undated file photo provided by U.S. Centers for Disease Control and Prevention shows the CDC’s laboratory test kit for the new coronavirus. (CDC via AP, File)
Maryland and Virginia saw the first people in the D.C. area tested for the new coronavirus. Those tested included a Maryland resident and a George Mason University student. However, the results came back negative.
For the new few weeks, health departments in D.C., Maryland and Virginia reported a trickle of new test results — all negative.
The World Health Organization declares the outbreak a global emergency after the number of cases worldwide spikes more than tenfold in a week.
The U.S. declared a public health emergency.
President Donald Trump signed an order that temporarily bars from the U.S. foreign nationals, other than immediate family of U.S. citizens and permanent residents, who have traveled in China within the last 14 days.

Workers pack bottles of alcohol disinfectant in a factory in Suining in southwest China’s Sichuan province Tuesday, Feb. 11, 2020. (Chinatopix Via AP)
The U.S. recorded its first coronavirus death: a man in his 50s at a long-term care facility in Washington state.
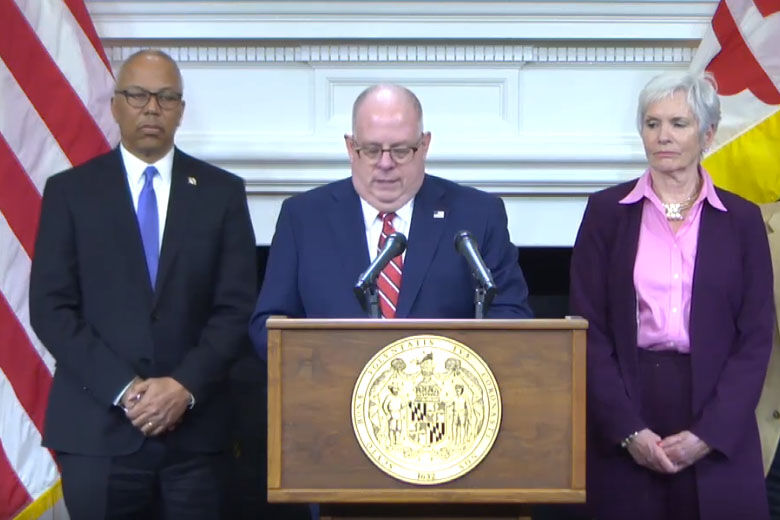
Maryland Gov. Larry Hogan announces the first three laboratory-confirmed cases of COVID-19 in the state of Maryland on March 5, 2020. The governor is flanked by Lt. Gov. Boyd Rutherford and Deputy Health Secretary Fran Phillips.
Maryland Gov. Larry Hogan announced three people in Maryland, all in Montgomery County, had tested positive for the virus — the first three known cases in the D.C. region. The first cases in the state included a married couple in their 70s and a woman in her 50s who had returned from a cruise along the Nile River.
Hogan announced a state of emergency.
Two days later, D.C. Mayor Muriel Bowser announced the first known coronavirus case in the District. The Rev. Timothy Cole, the rector of Georgetown Christ Church, had recently traveled to Kentucky for a church conference. Several other parishioners would later test positive amid a burgeoning outbreak.
That same day, Virginia also recorded its first case: a U.S. Marine stationed at Fort Belvoir.

Mayor Muriel Bowser speaks at a news conference to announce the first presumptive positive case of the coronavirus, technically known as COVID-19, in Washington, Saturday, March 7, 2020. (AP Photo/Patrick Semansky)
D.C.’s Mayor Bowser declared a public health emergency and urged all large gatherings planned in the District to be postponed or canceled. At the time, there were 10 confirmed coronavirus cases in D.C. — and more than two dozen in the broader D.C. region.
Health officials said there was evidence that community transmission of the coronavirus was occurring.
It was also on this date the WHO first characterized COVID-19 as a pandemic.
In a dramatic announcement, Maryland Gov. Hogan issued an order banning all large gatherings of people and activated the National Guard, while the state superintendent of education ordered all public schools in the state to close for two weeks.
Hogan’s announcement came after officials announced the first known case of a patient being infected with coronavirus through what’s known as community transmission.
That same day, Virginia Gov. Ralph Northam also declared a state of emergency.

Maryland Gov. Larry Hogan addresses reporters, March 16, 2020 in Annapolis. From left is Deputy Health Secretary Fran Phillips, Maj. Gen. Timothy Gowen, the adjutant general of the Maryland National Guard, Hogan, and Superintendent of the Maryland State Police Woodrow Jones. (AP Photo/Brian Witte)
Following Maryland’s move closing schools for two weeks, D.C. and Virginia announced schools would be closed through the end of March.
D.C.’s Bowser also issued a new order banning gatherings of 250 people or more in response to the spread of the virus. The mayor’s previous measure had been only a recommendation. The threshold would later be lowered to 10 people, in line with CDC guidance.
That same day, speaking from the White House, Trump declared a national emergency.
The region marked a sad milestone: the first coronavirus death in D.C., Maryland or Virginia.
Health officials said they weren’t sure how the James City County, Virginia, man in his 70s had contracted the virus, and they suspected the virus was spreading in the community.

A downtown Bethesda restaurant is closed as Maryland Gov. Larry Hogan’s executive order takes effect, closing bars, restaurants, gyms and movie theaters across the state in response to coronavirus. (AP/Manuel Balce Ceneta)
D.C.’s Bowser ordered all bars and restaurants in the District to operate as carryout and delivery only. In addition to restaurants, the D.C. Health Department said movie theaters, health clubs, spas, massage parlors and other large businesses also need to close.
Maryland’s Hogan issued a similar order.
The number of coronavirus cases around the region continued to climb, reaching more than 100.
At a White House briefing that day, Trump and members of his Coronavirus Task Force called on Americans to practice social distancing and to avoid gatherings for the next 14 days.
Maryland’s Hogan announced he was pushing back the state’s presidential primary, initially scheduled for April 28, until June 2. Under plans later put together by the state board of elections, the rescheduled primary will mostly be done by mail, but there will be one polling place open in each county.
Following the moves by Maryland and D.C. to close restaurant dining rooms and movie theaters, Virginia’s Northam issued an order enforcing a 10-person limit in restaurants and other businesses. He would later order entertainment venues closed entirely.
Maryland marked its first coronavirus death: A Prince George’s County man his 60s with an underlying medical condition.
At the time there were about 200 coronavirus cases in D.C., Maryland and Virginia.

Main Street in Annapolis is seen in this March 2020 photo. (AP Photo/Susan Walsh)
In a further clampdown on public gatherings, Maryland’s Hogan ordered all shopping malls and entertainment venues in the state to close. He also issued an order lowering the threshold on gatherings to 10 people or less, and promised it would be enforced by law enforcement.
Elsewhere, Italy overtook China as the country with the most coronavirus-related deaths at the time — more than 3,400 — and the governor of California issued a statewide order for people to stay home.
D.C.’s Bowser extended the closure of public schools through April 27. As it stands now, Bowser has yet to make a decision on when — or if — students will return to classrooms this school year.
In addition, Bowser extended her order banning dine-in services at restaurants and requiring them to operate on a takeout or delivery-only capacity through most of April.
That same day, D.C. also recorded its first death from COVID-19: a 59-year-old man.
In New York, which was soon to become the U.S. epicenter of the pandemic, the governor issued a “shelter-in-place” order, directing residents to stay home.

Virginia Gov. Ralph Northam gestures during a news conference at the Capitol Wednesday, April 8, 2020, in Richmond. (AP Photo/Steve Helber)
In another whirlwind of official pronouncements, Maryland’s Hogan ordered nonessential businesses in the state to close, and Virginia’s Northam ordered all public schools to keep their doors closed through the end of the academic year.
Earlier that month, organizers of the National Cherry Blossom Festival, usually one of the District’s marquee spring events, canceled most of the festivities.
At the time, there were more than 650 coronavirus cases in region.
Following Maryland’s earlier move, D.C.’s Bowser ordered nonessential businesses, such as salons, barbershops and clothing stores, in the city to close.
The Metro transit system, which had already announced service reductions, announced it was closing more than a dozen rail stations indefinitely. Ridership had fallen by 90% as many workers around the region worked from home.
By that point, the region recorded more than 800 coronavirus cases and 13 deaths.

A D.C. police vehicle is parked on the other side of a tape police line along the Tidal Basin as cherry blossoms cover the trees, in Washington, Monday, March 23, 2020. (AP Photo/Carolyn Kaster)
In Maryland, public schools, which were set to reopen at the beginning of April, were instead ordered closed through April 27, by order of state Superintendent of Education Karen Salmon. It’s still to be decided if students will actually return to classrooms this school year.
Meanwhile, the number of COVID-19 cases across Maryland, D.C. and Virginia continued to rise, totaling more than 1,000 cases.
Congress passed and Trump quickly signed an unprecedented $2.2 trillion economic rescue package into law.
The measure contains a plan to send stimulus checks to millions of Americans. However, D.C. leaders criticized the measure after it categorized the District as a territory and slated it to receive $700 billion less in direct aid than states.
D.C.’s Bowser called it an “injustice” and said she is continuing to work with congressional leaders to secure more money for the city.
Nationwide, the number of coronavirus infections surged past 100,000 and the number of deaths topped 1,500.
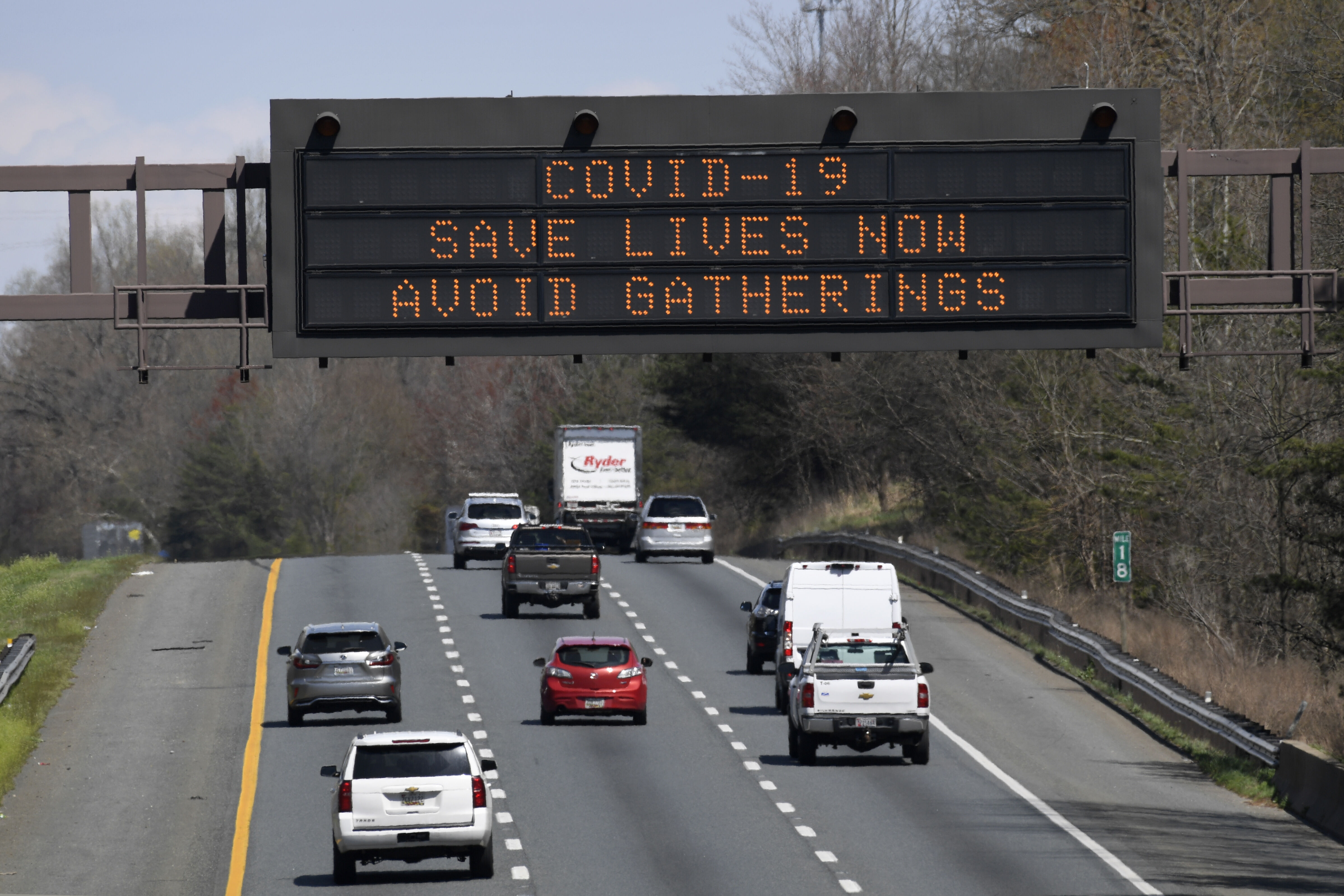
A sign about the coronavirus is displayed over U.S. 50 in Davidsonville, Maryland, Monday, March 30, 2020. (AP Photo/Susan Walsh)
In the most significant step taken to fight the spread of the virus, the leaders of Maryland, D.C. and Virginia issued formal “stay-at-home orders.”
All three orders were similar, directing residents to stay in their homes except for trips to the grocery store, to get medical care, going to work and outside recreation as long as social distancing guidelines were followed.
In all three jurisdictions, restaurants were allowed to stay open, offering takeout and delivery service.
The total number of coronavirus cases in D.C., Maryland, and Virginia hit more than 2,900, with 39 deaths.
Officials in D.C. unveiled a model of projected coronavirus infections that estimated up to 93,000 total infections in the District and deaths at anywhere from 225 to 1,000.
In Virginia, Northam said the state was “facing a recession” in the wake of the coronavirus response efforts, and he told state agencies to prepare for budget cuts.
The White House Coronavirus Task Force unveiled a new recommendation from the CDC: Americans should cover their faces with a cloth mask or other face covering when leaving the house, especially in places such as grocery stores where practicing social distancing is difficult.
Overall, coronavirus cases in D.C., Maryland and Virginia topped 5,500. The number of deaths reached more than 100.

Maryland Gov. Larry Hogan arrives for a news conference in Annapolis, Friday, April 10, 2020. (AP Photo/Susan Walsh)
In a first of its kind virtual session, the D.C. Council unanimously approved a major coronavirus relief bill.
Among other provisions, the legislation includes a citywide freeze on rent increases, mortgage-payment deferrals, an expansion of unemployment insurance and the mailing of an absentee-ballot application to every voter.
The legislative action came as an economic analysis by the city estimated $607 million in lost revenue from shuttered businesses and out-of-work residents. Bowser ordered District government agencies to freeze hiring and salaries.

A customer at a Giant grocery store in Alexandria, Virginia, wears a protective face mask while waiting in line at the checkout. (Courtesy Shannon Finney/shannonfinneyphotography.com)
D.C.’s Bowser issued a new order requiring grocery stores to limit the number of customers inside stores and requiring customers to cover their faces.
The total cumulative number of cases of COVID-19 in D.C., Maryland and Virginia grew to over 10,000, and 226 people had died.
Maryland’s Hogan announced he was ordering a statewide budget and hiring freeze, and warned of cuts after “worst-case scenario” projections showed a $2.8 billion revenue shortfall.
Earlier that day, Maryland’s top financial official had called the coronavirus pandemic “the worst public health crisis and most devastating economic catastrophe of our lifetimes.”
Trump, who had drawn alarm when he earlier said he hoped to “reopen” the country by Easter, announced a task force that would come up with a plan for “opening our country.”
By this time, 330 people had died in D.C., Maryland and Virginia, and the total number of coronavirus infections reached more than 13,000.
A growing number of counties in the D.C. area announced new rules requiring grocery store customers to wear face coverings while shopping.
Montgomery, Prince George’s, Anne Arundel and Charles counties in Maryland all announced new rules requiring face masks in stores and other public places.
By this point, more than 16,600 people in D.C., Virginia and Maryland had been infected with the virus, and more than 460 had died.
Maryland Gov. Larry Hogan issued an executive order requiring customers to wear face masks or face coverings inside grocery stores and other retailers throughout the state and on any form of public transportation.
In D.C., Mayor Muriel Bowser extended a series of mandates social distancing measures, including a stay-at-home order, the closure of nonessential businesses and public schools, and a ban on large public gatherings through May 15. Those measures were originally set to expire April 24.
And in Virginia, Gov. Ralph Northam extended an executive order closing recreation and entertainment businesses and banning large gatherings until May 8. The state’s stay-at-home order still runs through June 10.
The news came as the region marked its deadliest two days of the pandemic, so far. Maryland, alone, recorded 40 deaths each of the past two days. All told, the coronavirus had claimed more than 616 lives in D.C., Maryland and Virginia. The number of total infections stood at more than 18,700.
The Association Press contributed to this report.
Like WTOP on Facebook and follow @WTOP on Twitter to engage in conversation about this article and others.
Get breaking news and daily headlines delivered to your email inbox by signing up here.
Читайте также:


